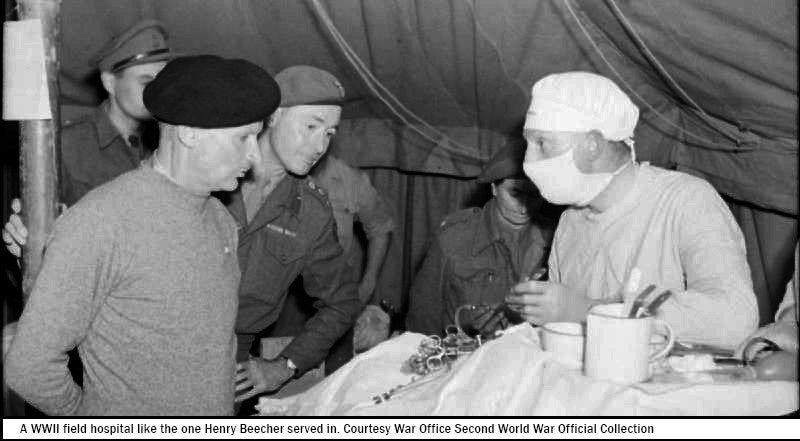
In a military field hospital during World War II a young doctor named Henry Beecher found himself in a desperate situation. He had run out of morphine and needed to perform surgery on a badly wounded soldier. Without hesitation one of the nurses filled a syringe with saline solution and gave the soldier a shot, just as if she were injecting him with morphine. The soldier calmed down and Beecher went ahead with the operation without anesthesia. The experience convinced him of the power of placebo and when he returned to the US after the war, he began to study the phenomenon. Henry Beecher’s wartime experiences would ultimately make him one of the most influential people on modern medical research.
This is a compelling story and it would have been a great way for me to start the chapter I’m currently writing about belief for my new book about evidence based mind body medicine... If it were true.
I have read the Henry Beecher World War II story countless times in news stories, popular books and even academic papers published in peer reviewed journals. It is usually used as proof of the power of belief in healing. In order to verify it I have read Beecher’s published papers, and been in contact with two academics and a librarian at Harvard who has access to Beecher’s personal archives. It turns out the story is not true. It is a fable, a legend, a myth. Likely a distortion of a real case study that Beecher published to demonstrate a very different point about pain and perception.
It is true that Beecher was an American anesthetist serving in the war. It is true that he had to treat a young solider, wild with pain from a wound to his chest. But Beecher had morphine on hand and could have given it to his patient. Instead, he chose to administer a sedative drug to calm the solider down. The Harvard trained doctor suspected that the young soldier’s pain was worsened more by his anxiety than the wound itself. The sedative worked.
Beecher used the case study to demonstrate that the severity of a soldier’s wound did not correlate with the severity of their pain. In his 1946 paper based on his observations of more than 200 gravely wounded soldiers in Africa and Europe, he found that three quarters of the badly wounded men he treated had so little pain that they declined morphine. Because their wounds signified a ticket off the front line and into the relative safety of the field hospital, Beecher thought that they perceived their pain differently.
A decade later he wrote a seminal paper called The Powerful Placebo which found that one third of people recovered directly because of their belief in a drug or treatment rather than the treatment itself. This paper has now been shown to have fundamental methodological errors, but nevertheless it carried great influence at the time and established the template for the process by which all new drugs are tested for the pharmaceutical industry today. It cemented Beecher as the founding father of the double blind, placebo-controlled method that is used as the gold standard for research today.
When you put Beecher’s work on placebo together with his work on pain in men wounded in battle, you start to see how the distorted story of surgery being performed under placebo anesthetic may have come about. The continued perpetration of the myth is an example of one of the major issues I am coming up against in my endeavors to investigate evidence based mind body medicine. There are a lot of so-called experts out there using half-truths, pseudo science and distorted anecdotes to make bold claims and justify dodgy treatments. There are also some credible scientists performing remarkable studies that carry significant implications for human health. It can be very difficult to navigate who’s who in the mind body zoo.
As someone who has wasted thousands of dollars on my health after being diagnosed with an autoimmune disease, these days it takes a lot to win my trust when I’m considering new information. I never make health decisions based on brief news reports where the story has been condensed. I loathe general sentences such as ‘research says’ or ‘scientists believe’ that don’t come with references or qualification. I rarely trust second hand interpretations of research findings unless they are being offered by a highly credible expert who weighs up all the available information. When I’m looking at someone’s bio, having the title ‘Dr.’ in front of their name doesn’t automatically mean they aren’t a quack. When I was researching my film The Connection, I acted on the advice of Harvard academic Anne Harrington, who wrote the book The Cure Within: A History of Mind Body Medicine, who recommended that if a person didn’t willingly discuss what their research/program/treatment doesn’t do then it might be wise to steer clear.
Given that the Henry Beecher anecdote is so widely used, I had thought it would take me about half an hour to verify. In the end, it took three days. While I’m thoroughly enjoying writing this book, there are times when I curse my ethics and wish I didn’t prioritize credibility so highly. Things would be a lot faster to write up if they didn’t need to be traced to the source. That said I know that the integrity of the research will mean that the book will ultimately end up being a resource that people can trust so I will continue along the path I’m on. Given that I’m already a month behind on my writing schedule, I’m hoping there won’t be too many more Henry Beecher’s along the way.




 My Year of Living Mindfully (DVD)
My Year of Living Mindfully (DVD) The Connection (DOWNLOAD-TO-OWN)
The Connection (DOWNLOAD-TO-OWN) My Year Of Living Mindfully - Book
My Year Of Living Mindfully - Book




